Sometimes parents and caregivers have a difficult time referring to a seizure type with the correct nomenclature. It is important to discover the exact type of seizures your loved one is having so that the correct treatment can be prescribed. Here is the link of videos of the different seizure types from Clinical Neurology Videos. These are for educational purposes only. Some of the videos require a Flash Player on your computer. It is also important that you track the quantity and type of seizures every day.
https://www.clinicalneurologyvideos.com/classification-of-seizures-videos
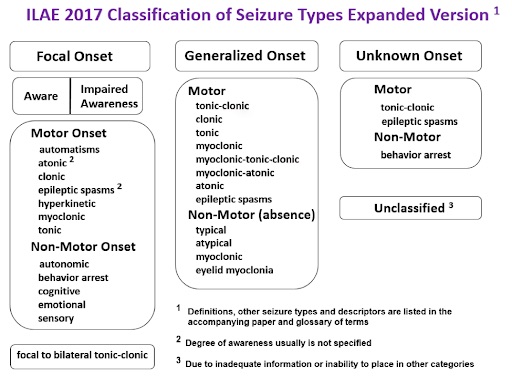
An internationally accepted system of classification separates seizures into two groups – “generalized” and “partial” (also called focal). The seizures associated with Doose syndrome are generalized. Generalized seizures affect the whole brain instantly, not just one part, and they alter consciousness. There is no warning.
Generalized seizures come in two forms; convulsive and non-convulsive. Non-convulsive refers to alterations of consciousness without jerking movements. Convulsive means that there are muscle movements like jerking or stiffening.
You may also encounter the terms “Clinical” and “Subclinical” in regard to seizures. Clinical seizures are those that can be observed physically. Subclinical seizures are those that show up on an EEG but don’t show up in a way that can be observed physically.
Doose syndrome is a complex seizure disorder that presents as a mixed bag of generalized seizure types. The myoclonic-atonic seizure (also called drop seizure or drop attack) is the core seizure type associated. All children with MAE will experience either myoclonic or myoclonic-atonic seizures – or both – but it is common for them to experience other generalized events including absence, atypical absence, myoclonic, tonic-clonic, episodes of non-convulsive status epilepticus (NCSE) and, in rare cases, tonic seizures.
Also, though not confirmed through any scientific study, many parents believe that once medicated, seizures can become more difficult to classify. As a result, some parents become convinced that their child has focal seizures and/or tonic seizures that may be typically generalized seizures that have been altered by the prescribed medication. To make matters more complicated Hermann Doose who identified this syndrome, noted that in regressed stages of Doose syndrome pseudo-focal seizures may appear (this is when the seizure looks focal ie: one part of the body, but the EEG shows it is generalized).
Below is a list of typical seizure types seen in Doose syndrome and their descriptions. This content is part of our “Doose Dictionary” which can be found in its entirety here.
Typically Present
Myoclonic
What happens?
Myoclonic seizures (myo meaning muscle, clonic meaning jerk) is a sudden involuntary contraction of muscle groups. In Doose syndrome, myoclonic jerks consist of symmetric, mostly generalized jerks, accentuated in the arms and the shoulders and frequently simultaneously with a head nod; both the arms may fling out together and simultaneously a head nod may occur. Sometimes the entire body may jerk, just like a startle response. As is the case with all generalized seizures, the child is not conscious during the event but the seizure is so brief that the person appears to remain fully conscious. The intensity of these seizures is variable and ranges from violent myoclonic jerks with sudden falls to mild abortive forms presenting simply as short irregular twitches or head nods.
The jerk arises from deep structures in the brainstem that control posture and tone in the body. A sudden increase in tone in a muscle group will cause a sudden movement of that part of the body. An abrupt increase in tone in the flexor muscles will cause the body to bend forward at the waist, the head to drop down on the chest, the arms to bend at the elbow or the knees to come up to the chest. An abrupt increase in tone in the extensor muscles will cause the head to be thrown back, the back to arch, the legs to extend, the arms to stiffen. Any or all of these movements may occur during a myoclonic jerk. If they occur while a child is standing, he may be suddenly thrown back to the ground, or he may suddenly be thrown forward to the ground, perhaps hitting his/her face, breaking a tooth, or causing a facial laceration.
Myoclonic-atonic (aka Myoclonic-Astatic)
The myoclonic-atonic seizure is rare and unique to MAE and is one of the most important and distinct features which helps distinguish it from other epilepsy syndromes.
Like myoclonic seizures, myoclonic-atonic seizures (also called atonic or drop attacks) are sudden, single events. Myoclonic-atonic seizures involve abrupt loss of muscle control causing the person to fall to the ground, often resulting in injury. For any family and child, the sudden, violent impact and resultant injuries are seen with myoclonic-atonic seizures make them one of the most frightening and distressing types of seizures to live with.
As the label myoclonic-atonic epilepsy (MAE) suggests, myoclonic-atonic seizures are the core seizure type associated with the disorder. In Doose syndrome, myoclonic-atonic seizures can be serious because they may be difficult to control, occur frequently daily putting the child at persistent risk of injury, and because they are only one manifestation of this mixed seizure disorder.
What happens?
Myoclonic-atonic seizures are sudden involuntary events like myoclonic seizures, however, rather than a sudden increase in muscle tone causing a jerk, atonic seizures involve a sudden loss of muscle tone.
Myoclonic-atonic seizures we see in Doose syndrome involve this atonic seizure (loss of muscle tone) often preceded by a short myoclonic (jerk) component as well. Arms, legs, or torso muscles that support the body by their tone, suddenly go limp; the body gives way with a jolt. The torso may slump, the legs may give way, or the body may fall to the ground. If a myoclonic-atonic seizure occurs while a child is standing, the seizure may cause the child to slam violently to the ground, perhaps hitting his/her face, breaking a tooth, or causing a facial laceration. Some describe this seizure as someone cutting the strings on a marionette puppet.
Like myoclonic seizures, atonic seizures arise from deep structures in the brainstem that control muscle tone. Since the areas that increase tone are close to those that decrease tone, children with seizures involving sudden changes in tone may have either myoclonic or atonic seizures and often both which is what we see typically with Doose syndrome.
As is the case with all generalized seizures, the child is not conscious during the event but the seizure is so brief that he/she usually recovers quickly. Sometimes a child may be mildly agitated or disorientated following an atonic seizure. If an injury has resulted, he/she may be duly distressed.
Often Present
Absence
Absence seizures can appear to observers as though the child is daydreaming or switching off, something we all do when our mind is wandering. Because absence seizures may be hard to distinguish from the child’s usual behavior, they may be difficult to detect. They can occur many times a day and are often mistaken for daydreaming.
In Doose syndrome, absence seizures occur in more than one-half of the cases. These absence seizures often accompany myoclonic seizures, especially clusters of myoclonic and / or myoclonic-atonic seizures. If these seizures occur frequently throughout the day, they can interrupt the child’s ability to function properly because his/her awareness (and the brain’s processing) is being constantly interrupted.
What happens?
Like all of the generalized seizures, an absence seizure starts suddenly and without warning. The child displays a glazed look and stares. Sometimes there is mild twitching of the mouth, eye blinking, or barely noticeable head bobbing which may give the observer a clue that seizure activity is occurring. The event usually lasts only seconds, sometimes 15-30 seconds or perhaps longer, and ends just as abruptly as it started. These events may be so brief that they are observable only on the EEG. When the seizure ends, the child is immediately alert and there is no confusion afterward. However, the child will have missed some of what is happening around him/her.
As is the case with all generalized seizures, the child is momentarily unconscious during the event so he/she doesn’t know what is happening, cannot recall anything, is unresponsive and no level arousal will bring them around until the seizure is finished.
Atypical Absence
Atypical absence seizures are similar to absence seizures but, as the name suggests, they are unusual or not typical. The child will stare, as with an absence seizure, but during an event, he/she will be somewhat responsive. Atypical absence seizures are similar to absence seizures but may have more pronounced motor symptoms such as tonic (stiffening) or clonic (jerking) spells or may have automatisms (involuntary behaviors) as seen in complex partial seizures. The EEG does not have the classic three-per-second spike and wave pattern seen in simple absence seizures. Like absence seizures, it can appear to observers as though the child is daydreaming or switching off so it may be hard to distinguish from the child’s usual behavior and therefore difficult to detect. They can occur many times a day and are often mistaken for daydreaming or look as though the child is zoning out or “not with it”.
In Doose syndrome, atypical absence seizures may be just one manifestation of this mixed seizure disorder. Atypical absence seizures often accompany clusters of myoclonic and/or myoclonic-atonic seizures. If these seizures occur frequently throughout the day, they can interrupt the child’s ability to function properly because his/her awareness (and the brain’s processing) is being constantly interrupted.
What happens?
Like all of the generalized seizures, an atypical absence seizure starts suddenly and without warning but the shift in consciousness may be so subtle that it may be very difficult for an observer to detect when the seizure starts or finishes. Similar to an absence seizure, the child displays a glazed look and stares. However, unlike a simple absence seizure, the child may be somewhat responsive and also have more pronounced motor symptoms such as twitching of the mouth, eye blinking, mild head bobbing which may give the observer a clue that seizure activity is occurring. As is the case with all generalized seizures, the child is momentarily unconscious during the event so he/she doesn’t know what is happening, cannot recall anything, but in the case of an atypical absence seizure, he/she may be somewhat responsive to and aware of his/her surroundings.
These events may be so brief that they are observable only on the EEG which will show a spike and wave pattern that distinguishes it from a simple absence seizure. Sometimes the events may last 15-30 seconds or perhaps longer and, to the observer, there may be an obvious change in the child’s state of consciousness. Being somewhat responsive during a longer event, the child may have delayed reactions, seem out of character, be easily confused or agitated. The “somewhat responsive” feature of an atypical absence seizure may lead an observer to mistake the event for a complex partial seizure. Sometimes the seizures may go completely unnoticed because the event is indistinguishable from the child’s usual behavior. When the seizure ends, the child is usually alert afterward however he/she will have missed some of what is happening around him/her.
Tonic-Clonic
Tonic-Clonic Seizures (formerly Grand Mal)
A generalized tonic-clonic seizure (GTC) is the sort most people think of when seizures are mentioned. Tonic-clonic seizures can be distressing to witness, especially when it is your child, but understanding what is happening does help us to cope with the situation.
In 60% of cases, the first seizure seen in Doose syndrome is a generalized tonic-clonic seizure and rarely the other types of generalized seizure (such as a myoclonic, myoclonic-atonic, or absence seizure). So, for most parents, a tonic-clonic seizure is the first symptom of MAE they will witness and it will strike completely out of the blue or sometimes accompany a fever.
What happens?
Initially, the child stiffens and simultaneously loses consciousness (so he/she is completely unaware of the event). Tonic (meaning stiff) refers to the stiffening stage and causes the child to fall to the ground. Typically, the eyes roll upwards, the head goes back, the back arches, and the arms and legs stiffen. The extension continues for what seems like a long time but rarely lasts more than thirty seconds. The brain cells are connected to other nerve cells through the spinal cord and during this tonic stage, all the muscles are contracted, including the chest muscles so it is difficult for the child to breathe. A combination of the face being flushed with the bluish blood of the veins and also the lack of oxygen causes the child to turn somewhat blue around the lips – a process called cyanosis. Excess saliva may cause a gurgling sound in the mouth or throat. The result of the muscles in the lungs contracting forces air out, sometimes making the child sound as though he/she is crying out. Occasionally, if the child’s bladder is full, he/she may lose bladder control.
After the tonic stage of a tonic-clonic seizure, the clonic (meaning jerk) phase of the seizure begins. The limbs jerk because now the muscles contract and relax in rapid succession. During this phase, the child may bite their tongue or the inside of their cheek. The fists are tightly clenched, the arms repeatedly flex at the elbows and then briefly relax. The legs flex at the hip and knee joint in a similar fashion; the head may flex and then fall backward. Initially, these movements occur rapidly but then gradually slow. The jerking becomes less intense and occurs at a slower rate, finally ceasing. Usually, a deep sigh signals the end of the jerking and normal breathing resumes.
The seizure is now over but the child is not awake and will not respond immediately. This recovery phase is called the postictal state when the brain can be thought of as exhausted from all its activity. The brain is quite active but its major activity is to inhibit (stop) the cells from firing. This inhibition has brought the seizure under control. This postictal stage or recovery time differs from child to child; it can last for a few minutes or longer, especially if the tonic-clonic seizure has been long. The child will probably feel like sleeping but can be roused and may feel tired, confused, agitated, or somewhat disorientated. Muscles will probably be sore. It is best to allow the child to rest until he/she is alert and fully recovered.
Non-Convulsive Status Epilepticus
There are two types of status epilepticus. One is the status epilepticus that most people think about, convulsive status epilepticus, in which the person is having prolonged tonic-clonic (convulsive) seizures which would be treated as a medical emergency. A separate type, non-convulsive status epilepticus (formerly referred to as “minor motor status”), is an episode when a person has prolonged absence and atypical absence events, lasting a half-hour, an hour, or days. This non-convulsive status (NCSE) is not life-threatening or brain-damaging but should be recognized and treated.
Fortunately, convulsive status epilepticus is not commonly associated with Doose syndrome. There is, however, a peculiar and rare type of non-convulsive status epilepticus common in Doose syndrome patients which may continue for hours or days if not interrupted by adequate measures without major consequences. NCSE is debilitating for the child and awful to witness as a parent but be reassured that it is not harmful.
Although many myths and fears persist about status epilepticus and non-convulsive status-epilepticus, with early recognition and appropriate treatment, children who experience episodes of status should return to their previous function and have no residual effects.
There is no evidence that spike-wave stupor seen with NCSE causes permanent damage to the brain, even when it goes on for hours or days. However, it disrupts the child’s level of function.
What happens?
By definition, NCSE is a long-lasting on/off absence seizure. Whereas an absence seizure lasts under a minute, episodes of NCSE can continue for a long time – thirty minutes, an hour, a day, or longer. Just like other generalized seizures, NCSE can start suddenly and without warning but the shift in consciousness may be so subtle that it may be very difficult for an observer to detect.
As is the case with all generalized seizures, the child doesn’t know what is happening during episodes of NCSE. Even though the child may be somewhat responsive and aware of the surroundings, he/she may only recall “snippets” of what happened or nothing at all. There is a lot of subclinical seizure activity occurring in the brain, constantly interrupting the child’s ability to process and function. As one child has described, things feel “fuzzy in the head”.
With non-convulsive status in MAE, the typical clinical picture is of a drowsy, stuporous (ataxic, or as if in a drunk state) child with subtle, barely detectable, myoclonic seizures often involving the face or extremities such as fingers. The child is unresponsive, drools has slurred speech or is non-verbal, and even immobile. This condition is termed by Doose syndrome parents as “full-blown NCSE”. If this situation continues for a long period it can be serious because it usually means that the child is immobile and non-verbal but, more importantly, unable to swallow. In this state, it is very difficult to keep fluids up regularly and take medication so if the NCSE cannot be stopped by adequate measures, hospitalization may be required. Fortunately, such a deterioration of conditions in Doose syndrome is rare.
Non-convulsive status in Doose syndrome can also be subtle and very difficult to detect without an EEG. Only a very careful history of an unexplained change in function or behavior can lead a treating doctor to suspect NCSE and to obtain an EEG. When dealing with MAE, parents, carers, and treating doctors should maintain a high index of suspicion that such changes in behavior may be an episode of NCSE especially if these events occur at a regular time every day. This milder condition is termed by Doose syndrome parents as “high-functioning NCSE”. Even “with a head full of seizures”, in this milder state of NCSE, parents are constantly amazed at what the child is capable of doing.
During an episode of “high-functioning NCSE”, as a parent, you might think that something is not quite right but not be able to put your finger on it. You may notice behavior that is out of character. These are some of the behaviors you might observe:
- somewhat unresponsive
- slurred or labored speech
- delayed actions (slow motion)
- decreased ability to “compute” (process/function) compared to normal
- grasping only “snippets” of his/her surroundings
- dream-like, sleepwalking state
- easily confused or agitated, or finds simpler tasks challenging
- subtle facial twitches or eye blinking, (a clue that seizure activity might be occurring)
- drooling which is out-of-character
You may suspect NCSE but the only way to know with certainty is to obtain an EEG during such an episode.
Rarer
Tonic
Tonic seizures are less common in Doose Syndrome and may suggest the need to re-evaluate the diagnosis with your neurologist. However, parents anecdotally tell us that sometimes after medication is initiated what looks like Tonic seizures may actually be other seizure types that have been altered by the effects of the medication. This can be a bit confusing. If you can catch one on video and have your neurologist evaluate it this could be helpful in differentiating between other types.
The unique nature of Tonic seizures come in the fact that they exhibit only stiffening and not a following clonic phase of a tonic-clonic. They are different from myoclonic seizures in that they exhibit stiffening for at least a few seconds as opposed to myoclonic which are quick jerks and don’t persist beyond a fraction of a second. Both tonic and atonic seizures can cause falls, though atonic seizures are the loss of all muscle tone where tonic is the sudden stiffening of the muscles.
What Happens?
Tonic seizures are brief seizures (usually < 60 seconds) consisting of the sudden onset of increased tone in the extensor muscles. If standing, the patient typically falls to the ground. These seizures are invariably longer than myoclonic seizures. The degree to which consciousness is impaired is often difficult to assess. In seizures lasting longer than a few seconds, impairment of consciousness is usually apparent. Postictal impairment with confusion, tiredness, and headache is common. The degree of postictal impairment is usually related to the duration of the seizure activity and is dramatically increased in tonic seizures.
Track your seizures
Tracking your loved one’s seizures is an important process and critical to discovering if the seizures are under more control with particular therapies. It is not uncommon for seizures to number in the hundreds a day, and for there to be multiple seizure types. Noticing that you are having 50 less seizures a day could be a 25% reduction and worth staying the course on a particular treatment. There are a lot of options. Some families choose a good old fashion notebook. Some transfer that information to an excel spreadsheet to share with their medical team, but most people use an app that is helpful to share, create graphs, and other diagnostic tools that may connect sleep, diet, medicines, or other culprits.
Seizure Tracker – allows for an extensive diary, graphs, detailed reports, and mobile access. (Android and IOS)
https://seizuretracker.com/
SeizAlarm – Is a user-friendly iPhone and Apple Watch app that allows those with epilepsy to alert emergency contacts automatically when seizure-like motion is detected or manually if they need immediate help or think they might need help soon.
http://seizalarm.com/
Overwatch Digital Health – Real-time seizure monitoring, alerting, and reporting. Connects with the Apple watch and downloaded app.
https://overwatchdh.com/